日本神戶大學姐妹校實習心得(102001070 醫學六 陳昱豪)
交換日期:2018/06/18~2018/07/15
見習科別:Dematology
Review of the program in Kobe University Hospital
In the first two weeks, I was in Dermatology. I haven’t run Dermatology in Taiwan yet, so it was my first time. I was glad that Dr. Fukunaga thought that I did better than the same grade of Japanese students.
In Kobe university hospital, I saw many rare cases including Madelung disease , SAPHO syndrome, AIGA and XPV which I think I will never have the chance to see in Taiwan if I only run the department for two weeks. I also saw many pemphigus and pemphigoid cases and Dr. Fukunaga didn’t know why there were so many bullous disease cases in this month. He even made a joke that maybe it was the season of bullous disease. The dermatologist here are very nice. They were willing to teach me, translate the Urticaria questionnaire into English for me and find English papers of AIGA when I needed it. In Taiwan, when we are in the outpatient clinic, the doctors usually won’t speak to us because of too many patients. Therefore, I learned a lot since nearly every patient Dr. Fukunaga explain his/her condition to me. In the conference on Tuesday, Dr. Fukunaga, Ken and Ono sensei sat next to me and explain the patients’ status to me and explain what the pathology of the biopsy is about.
Wednesday is surgery day. I was surprised then because I didn’t even know that dermatologists need to do surgery. I think in Taiwan dermatologists don’t have to do surgery because the training time of dermatologists in Taiwan is not as long as Japan. I saw the lipoma removal, condylomata removal surgery and Bowen disease surgery which required doing rhomboid flap.
According to Dr. Fukunaga, atopic dermatitis is the national disease of Japan, and fortunately there is new drug coming out. Its name is Dupilumab, an anti IL-4/13 antibody. An anti IL-31 drug specifically for itchy symptoms is also on trial now. The characteristic of atopic dermatitis is eczema which is heterogeneous. It may include erythema, papule, scale, and lichenification due to scratching. Instead, Psoriasis is more homogeneous with clear demarcated line and scale on it. I have learned so many things. However, since I spent most of the time in clinic, there wasn’t many pictures about what I learned due to the privacy of patients.
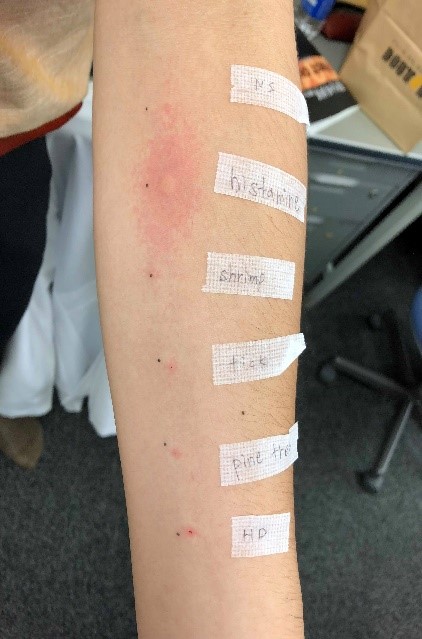
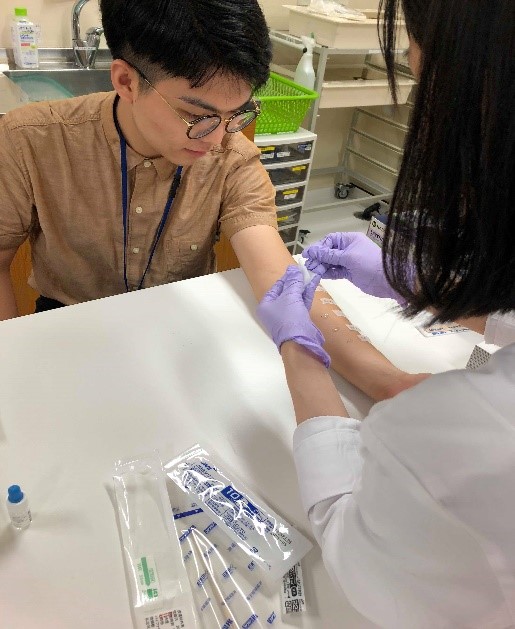
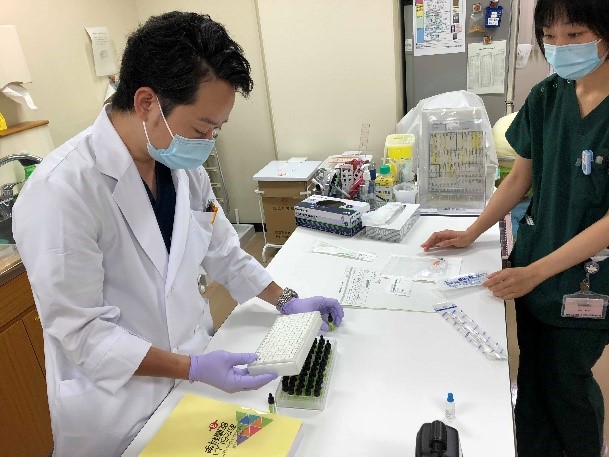
On Thursday, Dr. Imamura, let me do some procedure to the patient like applying SADBE to alopecia patients and iodine starch sweat test to patients suspected AIGA. I even did prick test on myself. The result is that I’m healthy. We can only see wheal on the site dripped with histamine which everybody will have the same allergy reaction.

Dr. Imamura also showed me around the environment of research building and teach me how to take small part of mouse tail and inject anesthesia to mice. I was afraid of catching mice, not to mention killing it. However, I guessed Dr. Imamura somehow pushed me to the limit. 



In the last two weeks I was in gastroenterology department. Unlike dermatology, I spend more time in endoscopy room than the clinic. The first time I entered the endoscopy room in Japan, I was surprised by the blue light in it. With the blue light, the endoscopy room totally seemed futuristic. Dr. Takao told me that though it is not evidence based, blue light is less likely to make people’s eyes tired than white light. I saw many ESD cases with doctors from Peru and Brazil. They told me that Dr. Toyokawa invented some tools for ESD and he is one of the best ESD doctors in the world. By using NBI and indigo carmine endoscopist could define the demarcated line of the lesion more easily. Then they marked the demarcated line by burning the mucosa and started to inject hyaluronic acid to detached the mucosa so it would be more easier to cut. Using a tool which was composed of clip and sling also helped cutting the lesion and pulled the lesion out after finishing cutting it. I think the lesion in esophagus is more difficult than in Gastric because unlike trachea having cartilage to maintain the shape, the muscle of esophagus squeeze together making it harder to mark the demarcated line.


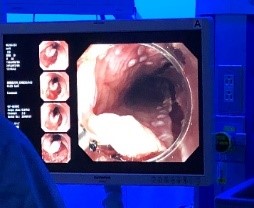
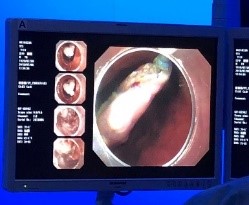

Other than ESD I also saw POEM (Peroral endoscopy myotomy) for Acalasia. The initial technique is similar to ESD. The endoscopist have to incise the mucosa and make a tunnel in submucosa. When reaching the tightest place of achalasia the space in submucosa became very small. However, after passing it, the space in submucosa suddenly became wide. This is how you know where the achalasia occurred. Then the endoscopist started to cut the circularis muscle under the mucosa until it’s under EC junction.
The difference of abdominal US between Taiwan and Japan is we don’t scan the prostate. However, it seems like scanning the prostate is a routine in Japan.
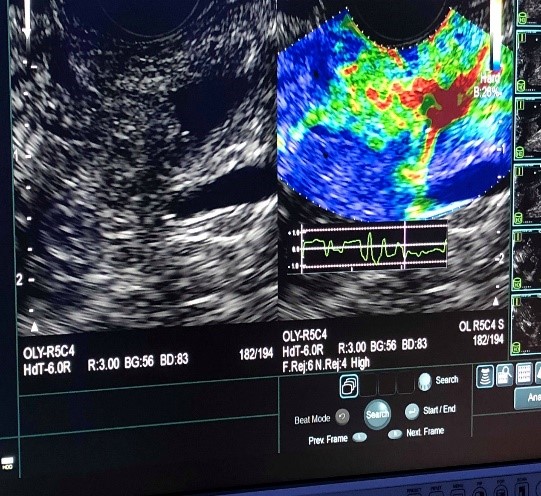
To distinguish the anatomy of EUS is way more difficult than normal abdominal US. The left side image below shows the EUS can detect the elasticity of the lesion to help doctors to differentiate whether it is tumor or not.
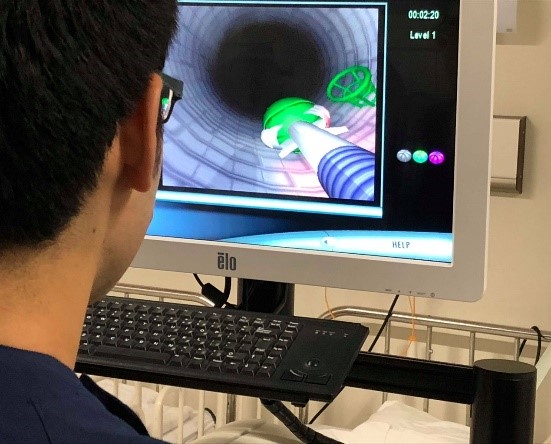
In the last week I finally had the chance to experience endoscopy simulator myself. Thanks Dr. Takao for giving me a one on one lesson. The students in Japan even had a competition on the game in the simulator called Endobasketball. I’m glad I’m at the sixth place among a hundred students. That gave me confidence of being a Gastroenterologist in the future.
There is no word can describe my appreciation for having a chance to be an exchange student in Kobe University Hospital. I really learned a lot and saw a lot. I have a great memory here that I will never forget.



